Stereotactic Radiosurgery (SRS) is a highly precise form of radiation therapy used to treat tumors and other abnormalities, primarily in the brain and spine, but also in other parts of the body. Despite the name "radiosurgery," it is a non-surgical procedure that does not involve incisions. Instead, it delivers intensely focused beams of radiation to a specific target area, minimizing exposure to surrounding healthy tissues.
SRS utilizes advanced imaging and planning software to deliver a high dose of radiation to a precisely defined target in one or a few treatment sessions. The process involves:
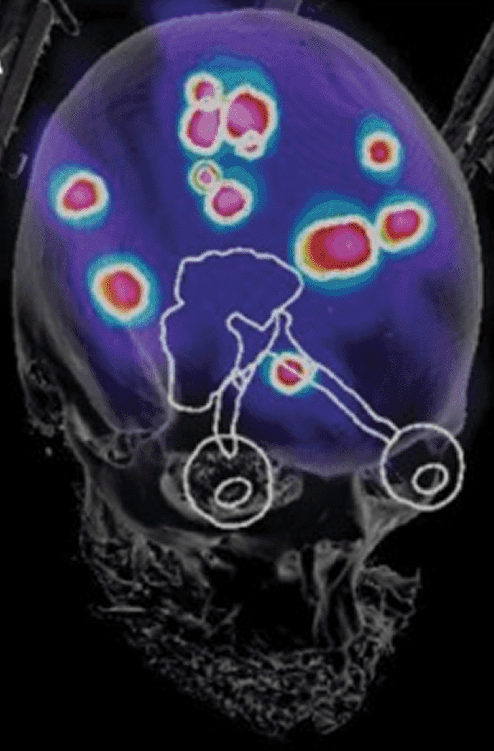
Detailed Imaging: High-resolution imaging techniques such as Magnetic Resonance Imaging (MRI), Computed Tomography (CT), and sometimes angiography are used to create a detailed three-dimensional map of the tumor or target area.
Treatment Planning: A multidisciplinary team, typically including a neurosurgeon, radiation oncologist, and medical physicist, uses specialized computer software to develop a customized treatment plan. This plan determines the optimal number, shape, and intensity of radiation beams, as well as the angles from which they will be delivered to converge precisely on the target.
Immobilization: To ensure the patient remains perfectly still during treatment, a method of immobilization is used. For treatments in the head, this often involves a rigid frame attached to the skull or a custom-molded mask. For body treatments, vacuum molds or other devices may be used.
Radiation Delivery: Using a specialized machine (such as a Gamma Knife or a linear accelerator-based system like CyberKnife), multiple radiation beams are directed at the target from different angles. Individually, these beams are low-intensity as they pass through healthy tissue. However, at the point where they intersect at the tumor, they deliver a very high, concentrated dose of radiation.
The high dose of radiation damages the DNA of the tumor cells, inhibiting their ability to grow and reproduce. Over time, this can cause the tumor to shrink or stop growing.
Acoustic neuromas, also known as vestibular schwannomas, are benign tumors that grow on the nerve connecting the brain to the inner ear (the vestibulocochlear nerve). SRS is a common and effective treatment option for acoustic neuromas, particularly for:
The primary goals of SRS for acoustic neuromas are to halt or slow tumor growth and to preserve the function of the hearing and facial nerves. While SRS does not remove the tumor, it can effectively control its size and prevent further damage to surrounding structures.
SRS is also used to treat a variety of other tumors and conditions in the brain and other parts of the body, including:
For these conditions, SRS aims to control the growth of the tumor or lesion, alleviate symptoms caused by compression or irritation of surrounding tissues, and preserve neurological function.
The SRS procedure is typically performed on an outpatient basis and involves several steps:
Benefits:
Risks and Side Effects:
Potential side effects are usually temporary and depend on the area being treated. They can include:
The decision to use SRS is made on an individual basis after a thorough evaluation by a multidisciplinary team, considering the specific type, size, and location of the tumor, as well as the patient's overall health and treatment goals.
To schedule your consultation, please use the form below. You could also do so by contacting the office directly by phone at (213) 262-8787, email at team@acousticneuroma.co, or visiting our offices at 415 N Crescent Dr, Suite 110, Beverly Hills, CA, 90210 and 1828 E Cesar E Chavez Ave, Ste 6200 Los Angeles CA, 90033.
Our Los Angeles-based surgical team, including Dr. Zachary R. Barnard, practicing at Cedars-Sinai Medical Center, Dignity Health Northridge Medical Center, and PIH Health Good Samaritan, and Dr. Kevin A. Peng at the renowned House Clinic serve both US-based and international patients.



We accept all insurances but contact us if you have further questions.