Glomus tumors, also known as paragangliomas, are a rare type of neuroendocrine tumor that arises from paraganglion cells. These cells are found in various locations throughout the body, but paragangliomas most commonly occur in the head and neck, particularly near major blood vessels and nerves. Common sites include the carotid body, the jugulotympanic area (near the ear and jugular vein), and along the vagus nerve.
While most paragangliomas are benign (non-cancerous) and slow-growing, they can cause significant problems by compressing or invading surrounding structures due to their location and vascular nature. A small percentage can be malignant (cancerous) and may spread to other parts of the body.
Diagnosis
Diagnosing glomus tumors involves a combination of evaluating symptoms, physical examination, imaging studies, and sometimes laboratory and genetic testing.
- Symptoms: Symptoms vary depending on the tumor's location.
- Head and Neck Paragangliomas (e.g., Jugulotympanic Glomus Tumors): Pulsatile tinnitus (hearing one's heartbeat in the ear) is a classic symptom. Other symptoms may include hearing loss, dizziness, facial weakness, hoarseness, difficulty swallowing, and a visible pulsating mass in the ear canal.
- Carotid Body Tumors: Often present as a slow-growing, painless mass in the neck. They may cause hoarseness or difficulty swallowing as they enlarge.
- Vagal Paragangliomas: Can cause hoarseness, difficulty swallowing, or vocal cord paralysis.
- Hormone-Secreting Paragangliomas: Although most paragangliomas do not secrete hormones, some can produce catecholamines (like adrenaline and noradrenaline). This can lead to symptoms such as high blood pressure, headaches, palpitations, excessive sweating, and anxiety.
- Physical Examination: A doctor may feel for masses in the neck or perform an examination of the ear, cranial nerves, and vocal cords depending on the suspected location.
- Imaging Tests: These are crucial for visualizing the tumor, determining its size and location, assessing its relationship to surrounding structures, and checking for multiple tumors or metastasis.
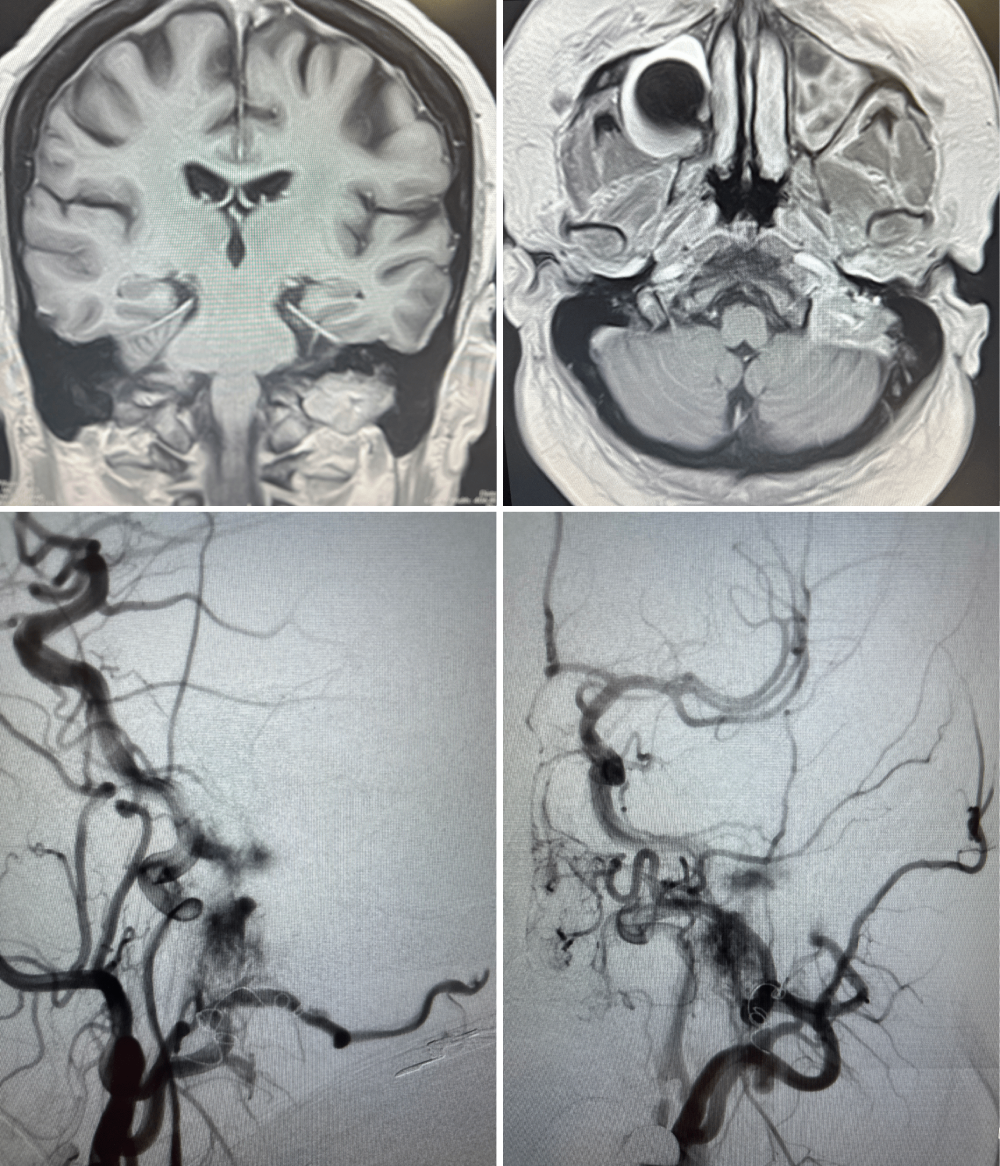
- MRI (Magnetic Resonance Imaging): Provides detailed images of soft tissues and is excellent for visualizing the extent of the tumor and its relationship to nerves and blood vessels.
- CT (Computed Tomography) Scan: Useful for evaluating the bony structures around the tumor and can show the tumor's enhancement pattern after contrast administration.
- Angiography: A procedure that involves injecting contrast dye into blood vessels to visualize the tumor's blood supply. This is particularly important for highly vascular glomus tumors and may be done as part of pre-treatment planning or embolization.
- Nuclear Medicine Scans (e.g., MIBG scan, DOTATATE PET scan): These scans can help identify hormone-secreting paragangliomas and detect tumors in other parts of the body.
- Laboratory Tests: Blood and urine tests may be performed to check for elevated levels of catecholamines or their metabolites, especially if a hormone-secreting tumor is suspected.
- Genetic Testing: Paragangliomas can be associated with inherited genetic syndromes. Genetic testing may be recommended, especially if there is a family history of paragangliomas or pheochromocytomas, multiple tumors, or if the tumor is diagnosed at a young age. Identifying a genetic mutation can have implications for the patient's prognosis, the risk of developing future tumors, and the screening of family members.
Treatment
The treatment of glomus tumors is complex and depends on several factors, including the tumor's location, size, growth rate, whether it is causing symptoms, if it is hormone-secreting, the patient's overall health, and the presence of multiple tumors or metastasis. Treatment decisions are often made by a multidisciplinary team of specialists, which may include surgeons (neurosurgeons, head and neck surgeons, otolaryngologists), radiation oncologists, endocrinologists, and geneticists.
Treatment options include:
- Observation (Watchful Waiting): For small, slow-growing, and asymptomatic tumors, particularly in older or less healthy patients, a "watch and wait" approach with regular imaging surveillance may be appropriate.
- Surgery: Surgical removal is a primary treatment option, especially for symptomatic or growing tumors. The goal is complete removal while preserving function of nearby nerves and blood vessels. However, surgery for glomus tumors can be challenging due to their high vascularity and proximity to critical structures. The type of surgical approach depends on the tumor's location. Potential risks of surgery include cranial nerve injury (leading to problems with voice, swallowing, or facial movement) and bleeding.
- Embolization: This minimally invasive procedure involves blocking the blood vessels that supply the tumor, usually performed by an interventional radiologist. Embolization can help reduce blood loss during surgery and may also be used to control tumor growth or alleviate symptoms in certain cases, sometimes as a standalone treatment.
- Radiation Therapy: Radiation therapy is an important treatment modality for glomus tumors, particularly for tumors that are large, inoperable, or when surgery carries a high risk of complications.
- Stereotactic Radiosurgery (SRS): As described previously, SRS delivers highly focused radiation to the tumor in one or a few sessions. It is often used for smaller to medium-sized glomus tumors, especially in the head and neck, to control tumor growth and minimize damage to surrounding nerves.
- Fractionated Radiation Therapy: This involves delivering radiation in smaller doses over several weeks. It may be used for larger tumors or when SRS is not suitable. Radiation therapy aims to stop or slow tumor growth, and while it may not cause significant tumor shrinkage, it can be very effective in achieving long-term local control.
- Medical Management: For hormone-secreting paragangliomas, medications (such as alpha-blockers and beta-blockers) are used to control blood pressure and other symptoms caused by excess hormones, especially before surgery or other interventions.
- Systemic Therapy: Chemotherapy or targeted therapies may be considered for malignant or metastatic paragangliomas, although these are less common treatment approaches for these typically slow-growing tumors. Peptide receptor radionuclide therapy (PRRT) is a specialized type of targeted radiation therapy that may be used for metastatic paragangliomas that express specific receptors.
Outcomes
The outcome for individuals with glomus tumors is generally favorable, especially for benign tumors that are completely removed. However, outcomes can vary depending on several factors:
- Tumor Location and Size: Tumors in critical locations or larger tumors are more challenging to treat and carry a higher risk of complications and potential long-term neurological deficits.
- Benign vs. Malignant: Malignant paragangliomas have a less favorable prognosis due to their potential to invade surrounding tissues and metastasize.
- Presence of Multiple Tumors: Individuals with inherited syndromes or multiple tumors may require ongoing management and face a higher risk of recurrence or developing new tumors.
- Treatment Modality: The choice of treatment and the skill of the medical team significantly influence the outcome.
- Hormone Secretion: Hormone-secreting tumors require careful medical management to control associated symptoms and reduce surgical risks.
Potential long-term outcomes and complications can include:
- Cranial Nerve Deficits: Depending on the tumor's location and treatment, there may be permanent weakness or paralysis of cranial nerves, affecting functions like hearing, balance, facial movement, voice, or swallowing.
- Recurrence or New Tumors: Even after successful treatment, there is a risk of the tumor recurring or new paragangliomas developing, especially in individuals with genetic predispositions. Long-term follow-up is essential.
- Vascular Complications: Due to their proximity to major blood vessels, there is a risk of bleeding or damage to these vessels during treatment.
- Effects of Hormone Secretion: If not adequately controlled, hormone-secreting tumors can lead to cardiovascular complications.
- Side Effects of Radiation Therapy: While SRS is precise, potential long-term effects can include changes in surrounding tissues or, rarely, the development of new tumors in the radiation field many years later.
Regular monitoring and a personalized, multidisciplinary approach to diagnosis and treatment are crucial for optimizing outcomes and managing the potential challenges associated with glomus tumors (paragangliomas).